by Todd Kenyon PhD CFA
COVID-19 death dashboards have become a fixture of daily television news broadcasts since March 2020. Whilst promoting daily death counters is unprecedented for any disease and clearly has deleterious effects on mental health, mortality trends may be the only accurate way to track the impact of the SARS-CoV-2 virus pandemic.
So-called cases and even hospitalizations are heavily influenced by testing rates and the most commonly used tests are unable to diagnose COVID-19 (they can only detect the presence of viral RNA; active or inactive). Yet even mortality statistics are highly uncertain – the WHO declares that a variety of factors lead to “a substantial lack of comparability between countries.” Attributing the true cause of death is far less straightforward than commonly believed, especially when it comes to COVID-19.
Some claim COVID deaths are undercounted. In developed countries, few all-cause deaths go unrecorded, so for those regions we assume the total fatality number is approximately correct. Hence, it is a question of fatality attribution – what was the underlying cause of death and was it correctly assigned? Recent articles claiming that COVID-19 deaths are under-reported don’t actually demonstrate significantly more fatalities directly due to COVID-19 disease. In fact they show that the collateral or “spillover” effects of lockdowns, fear, and isolation lead to significant fatalities from other causes. Here we present strong evidence that true COVID-19 deaths are significantly overcounted and over-reported by the media.
Cause of Death Attribution – A Difficult Process
Even during normal times, attributing Cause of Death (COD) is a murky process. It has been said that “using death certificates for anything beyond closing bank accounts is a disservice to society.” According to Joy Fritz, a former death certificate clerk:
- Natural cause of death (i.e., not trauma) reports exhibit a 20-60 percent inaccuracy rate according to the peer-reviewed literature. They are, by definition, medical opinions, not facts. (Study)(Study)(Study)
- Deaths in the elderly (the median age of COVID-19 mortality is 80+ in the UK for example) are frequently coded based on prescriptions taken or the condition they were admitted to a facility with or for. Deaths are frequently attributed to a “generic” cause like heart disease.
- There are strong bureaucratic incentives to not “rock the boat” in filling out COD on death certificates. Anything unusual or any uncertainty can result in long tie-ups and even trigger medical examiner requirements which can make the process more difficult for loved ones.
- Few deceased receive autopsies (4-8% in the US).
The pandemic has further increased the uncertainty in attributing COD due in part to the difficulty in distinguishing COVID-19 symptoms from other common respiratory illnesses. One study noted that “the symptoms may be similar to influenza or common cold” while another states that “neither absence or presence of signs or symptoms are accurate enough to rule in or rule out disease.” This does not mean that COVID-19 deaths were wrongly blamed on the flu, as flu cases effectively disappeared worldwide once SARS-CoV-2 got rolling. So if anything, nearly every respiratory-related death was labeled COVID-19. The CDC has a wide range of mortality estimates for common flu/pneumonia, varying up to 3-fold. So even with such a familiar illness, mortality estimates are just that: very rough estimates. The solution for COVID-19 was to use widespread incessant testing to track the pandemic, but this too was a massively flawed process.
PCR Test Determines COD
The inappropriate crutch of relying on PCR tests as an indicator of infection (in lieu of clinical diagnosis) underpins much of the flawed data reporting throughout the pandemic. Until mid-August 2020, if a deceased person in the UK had ever tested positive, they were recorded as a COVID-19 death. Even without a positive test, COVID-19 could be declared as the COD. The ONS declared in March 2020:
“It will be based on mentions of COVID-19 on death certificates. It will include suspected cases of COVID-19 where someone has not been tested positive for COVID-19.”
In August, the terms were changed to any positive test within 28 days of death, yet the ONS still clung to 60 days. Again, a positive test in no way indicates that the patient is sick with COVID-19 (the illness caused by the SARS-CoV-2 virus). Viral remnants and hence positive tests can persist for several weeks or months post infection. Even if the person was never infected with SARS-CoV-2, PCR tests can flag them positive for a variety of reasons. An asymptomatic or mildly symptomatic person may test positive, yet clearly if death occurs, it cannot reasonably be attributed to COVID-19. A positive test 4 weeks before an elderly terminal cancer patient passes away is clearly no basis for declaring they died due to COVID-19.
The WHO’s Broad Definition of COVID Deaths
The WHO guidelines also make it quite easy to attribute deaths to COVID-19:
“A death due to COVID-19 is defined for surveillance purposes as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g., trauma). There should be no period of complete recovery from COVID-19 between illness and death. A death due to COVID-19 may not be attributed to another disease (e.g., cancer).”
Note here that only alternative COD’s that cannot be associated with COVID-19 (a very short list) absolutely disqualify COVID. A patient suffering from terminal cancer who died within range (28 or more days) of a positive test or had broadly COVID-like symptoms, would be flagged as dying from COVID-19 – not cancer. In essence, it is difficult not to attribute deaths to COVID-19 when the guidelines are so wide-ranging as to include: a positive test weeks prior to death without proof of infection; vaguely suspicious symptoms without test confirmation; and death not directly attributed to COVID-19.
Again, recall the median age of death attributed to COVID-19 is 80+ and on average those deceased in the US had 2.9 comorbidities. The weakened elderly frequently suffer from (and succumb to) any number of respiratory illnesses on top of these comorbidities, so it’s easy to see that nearly every elderly death could be attributed to COVID-19 under these conditions.
Fatality Stats Reduced Significantly
Several examples demonstrate what can happen when death certificates are reviewed. Alameda County in California dismissed 25% of their previously recorded COVID-19 deaths because they were “clearly not” caused by COVID-19. And these were just the extremely obvious fatalities (e.g., trauma). The standard originally used by the county was “anyone who died while COVID-19 positive.” Note that this is likely more stringent than the jurisdictions who count positive tests up to months before death. The remaining 75% still included fatalities where “COVID could not be ruled out” but where there was no clinical evidence that the person died due to COVID-19. A second county in California uncovered similar results. Similarly, Massachusetts recently reviewed its nursing home deaths, resulting in reported total deaths “from” COVID-19 dropping 39%. Two regions in Sweden (where anyone with a positive test within 30 days of death is considered a COVID death) reviewed death certificates and found only 15-17% were decisively due to COVID, while 8-15% were wholly unrelated to COVID. In the remaining 70-75% COVID was a “contributing factor” but the patients were all sickly/frail with a mean age of 86-88. A recent court ruling in Portugal claims that only 0.9% of “COVID-19 deaths” were “verified”. While this claim remains to be substantiated by outside parties, the implications are clear. In general, standards for attributing deaths in the US vary widely from state to state, just as they do from nation to nation.
Double Standard
Recent direct communications from CDC researchers confirm the difficulty of accurately attributing death to COVID-19. When looking for COVID-19 deaths due to vaccine “breakthroughs”, the CDC removes any vaccinated patients who test positive but clearly did not die from COVID-19; e.g., trauma or delivery patients (much like the WHO guidance). Of the remaining vaccinated patients who test positive and die, the CDC also ignores asymptomatic patients because “they were unlikely to be hospitalized due to COVID-19 if asymptomatic.” This is a common sense method hitherto ignored worldwide when attributing cases, hospitalizations and deaths for COVID. Of the remaining vaccinated patients who die and have a positive test, the CDC marks them “unknown”, because they say “it is challenging to determine the relationship between a SARS-CoV-2 infection and the reason a person was hospitalized or passed away.” Imagine if this were how we treated all hospitalizations and deaths over the past year – the numbers would be far lower.
Furthermore, while there is a strong incentive in general to avoid bureaucratic red tape when declaring COD on death certificates, there are other powerful incentives in some countries to specifically list COVID-19 as the primary COD. In the US, hospitals were paid significantly higher medicare rates for treating COVID-19 patients – 2 to 3 times the amounts paid for typical respiratory illnesses. While few claim that practitioners set out to deliberately game the system, it incentivises COVID-19 designation which carries over, unchallenged, to death certificates. In addition, the Federal Emergency Management Agency provides a $9000 death benefit to surviving families if COVID-19 is listed as the COD, potentially silencing families who might otherwise think that the cause of death was not COVID.
Excess Mortality – More Than COVID
It should be clear by now that attributing fatalities to COVID-19 is a convoluted process rife with misaligned incentives. The antidote may be to look at “excess fatalities” – how many more people died versus what would typically be expected. However, we cannot just assume that all excess deaths in 2020 were due to COVID-19. Lockdowns, isolation, and general fear among the public certainly contributed to deaths from despair, suicides, missed medical treatments/screenings, and substance abuse to name but a few. For example in the US, the CDC shows that there were many thousands of excess deaths due to heart attacks and other “circulatory” causes in 2020. While some of these may have been complications from COVID-19, calls to emergency services and visits to ERs dropped significantly during the pandemic peaks. Hence, many of these are people avoiding treatment for heart attack and stroke symptoms due to fear. Dementia was another “excess” killer in 2020 with many thousands more deaths than expected, probably resulting from neglect and isolation.
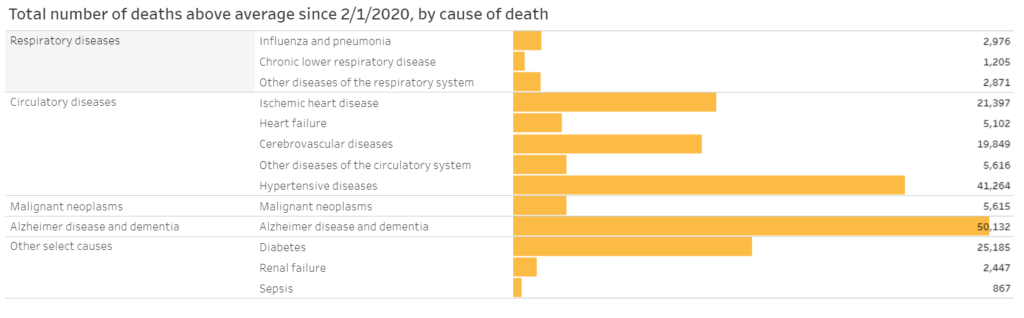
US data, Source: CDC
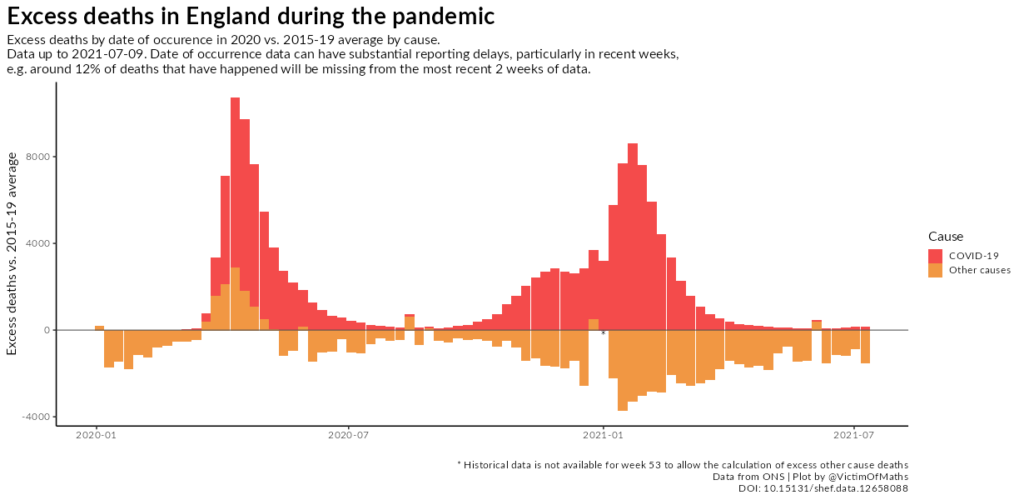
In the UK during the Winter 2020/21 wave, excess mortality attributed to COVID was mirrored by less than expected mortality from causes other than COVID. Clearly this implies that deaths from other causes were attributed to COVID.
Excess mortality in 2020 is also skewed for another reason: many regions suffered up to two complete “flu seasons” (in this case SARS-CoV-2 seasons) in one calendar year. It is normal for respiratory viruses to peak early in the calendar year in northern climates – a pattern repeated annually. Yet with SARS-CoV-2 we observed 2 peaks (or nearly so) within one calendar year in many regions likely due to the late start of the pandemic, relative to normal Corona virus seasonality.
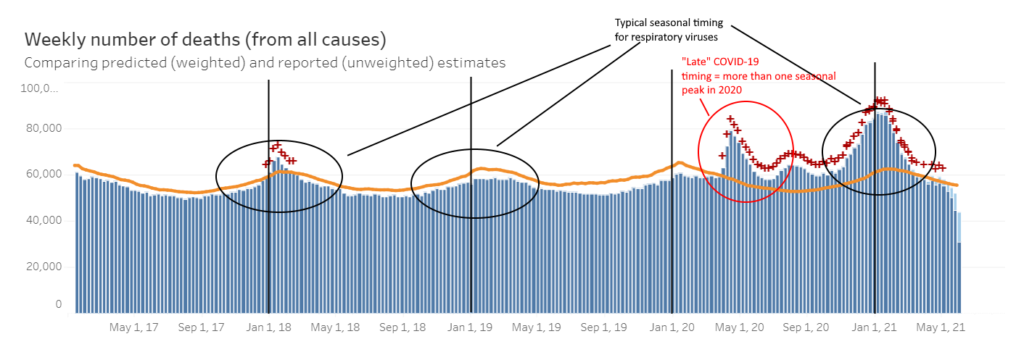
US data. Source: CDC, author’s interpretation
Years of Life Lost
Regardless of the exact mortality count, the Infection Fatality Rate of COVID-19 is now estimated to be ~ 0.15%, akin to common flu, which has never triggered the draconian response that COVID-19 has unleashed. Furthermore, while every death is tragic, the loss of a child is far more so in terms of lost life-years than an individual already close to the end of life. Thankfully, COVID-19 spares the young. Finally, we won’t know the full story until “pull forward” effects play out in the form of reduced mortality in future seasons due to the reduction of exceptionally large vulnerable populations in 2020.
As always, scientists should strive to report and analyze pandemic data accurately, whether it agrees or disagrees with their preferred hypothesis. There is little evidence indicating that COVID-19 fatalities in developed countries were attributed to other conditions. When one considers the lax COD standards, inappropriate tests and incentives to attribute fatalities to COVID-19, it is difficult to see how and why under-attribution would occur. Without accurate accounting of the severity of the disease, we cannot fairly evaluate the cost-benefit of public health policy (perhaps one reason good data is so hard to obtain). We question COVID-19 fatality attribution practices and hence the reported COVID-19 fatality numbers for just this reason. Without good data, good policy cannot be produced.
Photo by Krissana Porto on Unsplash
Todd brings a wealth of knowledge and a range of expertise to the PANDA panel. He has a PhD in Marine Biology, a BS in Mechanical Engineering, is a Charted Financial Analyst and a patented inventor and entrepreneur. Todd has a keen interest in endurance and water sports.