INFOBANK
MASKS
There is very limited research on the effectiveness of masks or the potential harms of their prolonged use in the general public.
The available literature indicates little scientific evidence that mask-wearing among the general public curbs disease spread. There is mounting evidence for the potential harms of mask wearing. Recent reviews and studies are summarized here.
MASK INEFFECTIVENESS
Physical interventions to interrupt or reduce the spread of respiratory viruses
Systemic Review by Cochrane
78 Randomized Control Trials were reviewed with 6 new trials conducted during Covid-19
“Wearing masks in the community probably makes little or no difference to the outcome of influenza‐like illness (ILI)/COVID‐19-like illness compared to not wearing masks.”
“The use of N95/P2 respirators compared to medical/surgical masks probably makes little or no difference for the objective and more precise outcome of laboratory‐confirmed influenza infection.”
(Jefferson et al., Jan 2023)
Non-pharmaceutical measures for pandemic influenza in non-healthcare settings—personal protective and environmental measures
Policy Review by Centers for Disease Control and Prevention
“We did not find evidence that surgical-type face masks are effective in reducing laboratory-confirmed influenza transmission, either when worn by infected persons (source control) or by persons in the general community to reduce their susceptibility.” (Xiao et al., May 2020)
Advice on the use of masks in the context of COVID-19
Interim Guidance by The World Health Organisation
“At present, there is no direct evidence (from studies on COVID-19 and in healthy people in the community) on the effectiveness of universal masking of healthy people in the community to prevent infection with respiratory viruses, including COVID-19.” (WHO, June 2020)
Physical interventions to interrupt or reduce the spread of respiratory viruses
Systemic Review by Cochrane
“The pooled results of [67] randomised trials did not show a clear reduction in respiratory viral infection with the use of medical/surgical masks during seasonal influenza. There were no clear differences between the use of medical/surgical masks compared with N95/P2 respirators in healthcare workers when used in routine care to reduce respiratory viral infection.” (Jefferson et al., November 2020)
Masking lack of evidence with politics
Review by The Center for Evidence-Based Medicine, University of Oxford
“It would appear that despite two decades of pandemic preparedness, there is considerable uncertainty as to the value of wearing masks.” (Jefferson & Heneghan, 2020)
Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers
Randomized control trial reveals a non-statistically significant difference between two groups of participants, one requested to wear a mask, the other not wearing a mask. “masks would not be effective against spread via aerosols, which might penetrate or circumnavigate a face mask” “The data were compatible with lesser degrees of self-protection.” (Bundgaardet al., March 2020)
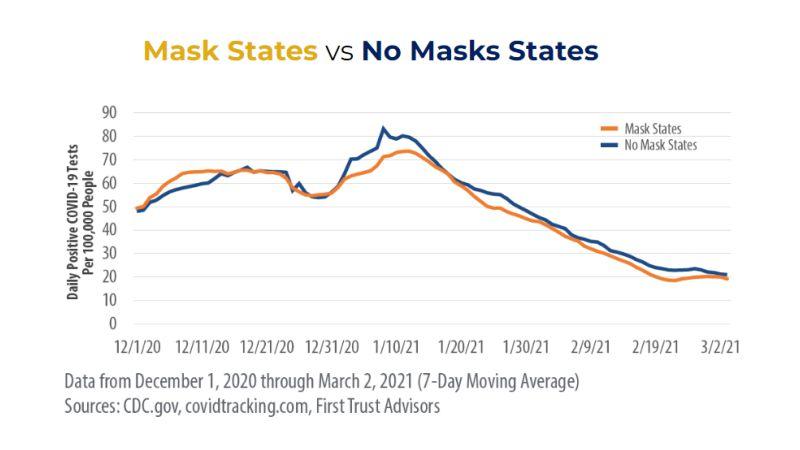
Mask mandate and use efficacy in state-level COVID-19 containment
“Case growth was not significantly different between [mask] mandate and non-mandate states at low or high transmission rates, and surges were equivocal.” (Guerra & Guerra, May 2020)
COVID-19 mitigation measures in primary schools and association with infection and school staff wellbeing: an observational survey linked with routine data in Wales, UK
“There was no evidence that face coverings, 2-metre social distancing or stopping children mixing was associated with lower odds of COVID-19 or cold infection rates in the school.” (Marchat et al., 2021)
Revisiting Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements—United States, July 1—October 20 2021
“We failed to establish a relationship between school masking and pediatric cases using the same methods but a larger, more nationally diverse population over a longer interval.” (Chandra & Høeg, 2022)
Evidence for Community Cloth Face Masking to Limit the Spread of SARS‐CoV‑2: A Critical Review
“The available clinical evidence of facemask efficacy is of low quality and the best available clinical evidence has mostly failed to show efficacy, with fourteen of sixteen identified randomized controlled trials comparing face masks to no mask controls failing to find statistically significant benefit in the intent‐to‐treat populations.”
“The primary mode of transmission (aerosol vs. droplet) for viral respiratory infections, including SARS-CoV-2, is controversial and remains unclear. If aerosol transmission plays a substantial role, the ability of masks to serve as a physical barrier to droplets becomes a less reliable surrogate of efficacy, since air expelled from the lungs necessarily penetrates the mask or flows around its edges, potentially advecting aerosols along with it” (Liu et al., 2021)
MASK FACTS
Several factors influence the effectiveness of cloth and surgical masks including their pore size and the extent of leakage.
Virus size vs mask pore size
The SARS-Cov-2 virus is so small, it can pass through the pores of the mask.
SARS-CoV-2 virus has a diameter of ≃ 0.1 microns = 0.0001 mm
The cloth mask pore diameter is ≃ 80-500 microns.
The surgical mask pore diameter is ≃ 13-585 microns. “A typical blue surgical mask has a median pore size of 19.3 microns”
Even if the mask layers can capture the large droplets, the virus can still pass through the pores with every breath.
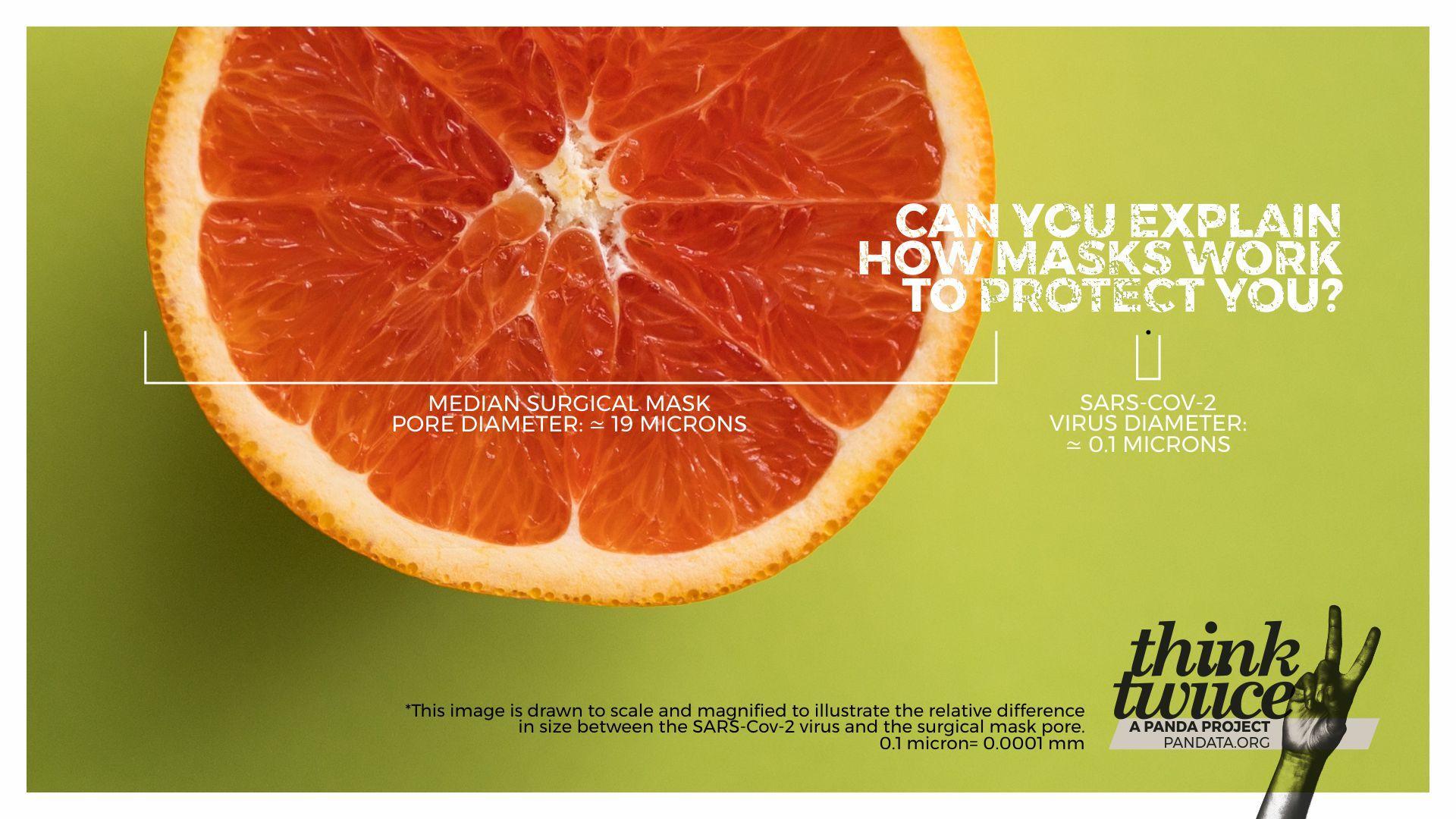
This image is drawn to scale and magnified to illustrate the relative difference in size between the SARS-Cov-2 virus and the surgical mask pore.
Mask leakage
Both cloth masks and surgical masks allow for high amounts of leakage rendering them completely useless for stopping transmission as SARS-CoV-2 is an airborne virus that spreads mainly via minute aerosols floating in the air.
Watch the video to see for yourself.
Mask effectiveness by Dr Byram Bridle (Associate Professor of Viral Immunology at the University of Guelph in Canada): Do Masks Work?
MASK HARMS
Mask use in the context of COVID-19
Interim Guidance by the WHO
The WHO lists mask disadvantages: discomfort, headaches, breathing difficulties, self-contamination, facial lesions, a false sense of security and poor compliance, difficulty with communication, among others (WHO, December 2020).
“Several studies have demonstrated statistically significant deleterious effects on various cardiopulmonary physiologic parameters during mild to moderate exercise in healthy subjects and in those with underlying respiratory diseases.” (WHO, December 2020).
Corona children studies “Co-Ki”: First results of a Germany-wide registry on mouth and nose covering (mask) in children
“Impairments caused by wearing the mask were reported by 68% of the parents. These included irritability (60%), headache (53%), difficulty concentrating (50%), less happiness (49%), reluctance to go to school/kindergarten (44%), malaise (42%) impaired learning (38%) and drowsiness or fatigue (37%).” (Schwarz et al., April 2021).
Carbon dioxide rises beyond acceptable safety levels in children under nose and mouth covering: Results of an experimental measurement study in healthy children
“We measured 13,100 ppm (SD 380) under surgical mask and 13,900 ppm (SD 370) under FFP2 [N95] mask in inhaled air.” “We measured 2,700 ppm (SD 100) CO2 at pre-baseline and 2,800 ppm (SD 100) at post-baseline. Appropriate contrasts revealed that the change was due to the masks only and the difference between the two types of masks was small and not significant. Wearing of NMC (surgical masks or FFP2 masks) raises CO2 content in inhaled air quickly to a very high level in healthy children in a seated resting position that might be hazardous to children’s health.” (Walach et al., 2022)
Contamination by respiratory viruses on outer surface of medical masks used by hospital healthcare workers
“Commonly isolated viruses from masks samples were adenovirus (n = 7), bocavirus (n = 2), respiratory syncytial virus (n = 2) and influenza virus (n = 2). Virus positivity was significantly higher in masks samples worn for > 6 h.” “Respiratory pathogens on the outer surface of the used medical masks may result in self-contamination. The risk is higher with longer duration of mask use (> 6 h) and with higher rates of clinical contact [contact with patients].” (Chughtai et al., 2019).
Non-targeted analysis of unknown volatile chemicals in medical masks
“12 high-risk volatile chemicals in medical masks were listed. This study could serve as a reference for identifying unknown substances and a guide for monitoring volatile chemicals in masks and promoting chemical safety improvements in products.” (Liu et al., 2022)
Parent Initiative
Concerned parents sent 6 face masks worn by their children to the University of Florida Lab for analysis of contaminants. This report, prepared by Jennifer Cabrera in June 2021, details the findings.
“The analysis detected the following 11 dangerous pathogens on the masks: Streptococcus pneumoniae (pneumonia), Mycobacterium tuberculosis (tuberculosis), Neisseria meningitidis (meningitis, sepsis), Acanthamoeba polyphaga (keratitis and granulomatous amebic encephalitis), Acinetobacter baumanni (pneumonia, bloodstream infections, meningitis, UTIs—resistant to antibiotics), Escherichia coli (food poisoning), Borrelia burgdorferi (causes Lyme disease), Corynebacterium diphtheriae (diphtheria), Legionella pneumophila (Legionnaires’ disease), Staphylococcus pyogenes serotype M3 (severe infections—high morbidity rates), Staphylococcus aureus (meningitis, sepsis)”.
For further information, please visit: